
Why Every Clinician Treating Low Back Pain Needs a Structured Core Assessment Framework
Why does low back pain persist despite good treatment? Learn how a structured framework for assessing core dysfunction improves clinical reasoning and patient outcomes.

The Overlooked Role of Sleep in Pain, Healing, and Nervous System Regulation: What Every PT Should Know
Discover how sleep physiology impacts pain, tissue healing, neural recovery, and patient outcomes. Learn why physical therapists must screen for, and address, sleep disruptions as part of comprehensive care.

Seeing What Isn’t There: Apophenia and the Art (and Science) of Physiotherapy
Explore how apophenia—our tendency to see patterns where none exist—shapes patient beliefs, therapist bias, and decision-making in physiotherapy, and how clinicians can harness it ethically to improve rehab adherence and outcomes.

Pelvic Health, Female Athletes & Performance: What If Our Model Is Wrong?
Explore why traditional pelvic health models may fall short for female athletes and how a holistic, evidence‑informed approach supports performance and symptom resolution.

Reframing Pelvic Health: Why the Biopsychosocial Approach Changes Everything
Discover how the biopsychosocial approach transforms pelvic health care. Learn practical strategies from Carolyn Vandyken and her 2026 mentorship program.

Optimize Your Clinic Workflow: New and Improved Calendar Features on Embodia
Discover Embodia’s latest clinic scheduling update, including a collapsible sidebar, full-screen calendar view, and powerful EMR scheduling tools. Learn how Embodia’s practice management calendar helps healthcare clinics schedule smarter with a new full-screen view and advanced features.

Is Concussion Rehab Really as Complex as It Seems?
Discover practical, evidence-based strategies for physiotherapists managing concussion in private practice. Learn how to build confidence, navigate evolving guidelines, assess key impairments, and collaborate effectively within an interdisciplinary team to support patients with persistent post-concussion symptoms.

Are Post-Traumatic Headaches and Concussions the Same Thing?
Learn how post-traumatic headaches differ from concussions, the types of trauma-related headaches, and why rest may not always be the best treatment.

Evolving Pelvic Health Care: Why a Biopsychosocial-Spiritual Approach Is Essential—And How to Integrate It Into Practice
Discover why nociplastic pain and modern pain science are reshaping pelvic health practice. This blog highlights insights from Carolyn Vandyken and invites you to her upcoming webinar on BPSS assessment and treatment.
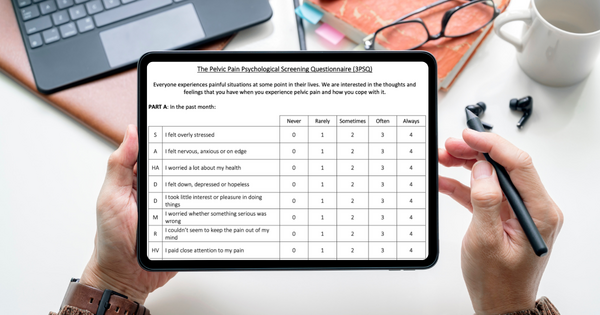
Embracing a Biopsychosocial Approach in Pelvic Health: Introducing the 3PSQ and Fre-PAQ
Explore a holistic, patient‑centered biopsychosocial approach to pelvic health — featuring two new tools for screening: the 3PSQ for psychological distress and the Fre‑PAQ for sensory‑motor dysregulation.

How to Turn Down the Volume on Persistent Pain A Practical, Neuroscience-Informed Approach for Physiotherapists
Learn how to help patients understand and manage persistent pain by turning down its volume through brain-based education and whole-person strategies.

Unlocking Movement Potential: Feldenkrais Method for Better Motor Learning
Integrate neuroscience and mindful movement. Discover how Feldenkrais principles elevate motor learning and rehabilitation in physiotherapy.